Facilities
Senior Behavior Wellness vs Medicaid
Medicare Coverage
Nursing homes that rely the most on Medicaid tend to have the hardest time providing adequate care for their residents-not just the people covered by the program but also those who pay privately or have traditional Medicare coverage. This is due to multiple factors:
- Reimbursement can be 45% less than traditional Medicare so clinicians are less incentivized to see these residents.
- IL Medicaid limits services provided for psychiatry and does not reimburse psychological services.
- Many Medicaid replacement plans require preauthorization for care and is time consuming and difficult to obtain.
- Payments take inordinately long to receive (sometimes greater than 6 months).
- Facilities with a high Medicaid population have less staff available to care for needs of residents due to low per diem rates and, as result, care suffers.

2018 CDC Facts
The Centers for Disease Control and Prevention (CDC) report that as of 2018 there were 15,600 licensed nursing homes in the U.S., 1.7 million nursing home beds, and 1.5 million nursing home residents.
Mental Illness Rates
In addition, up to 25% of all new admissions to a nursing home have a history of mental illness. This clearly indicates a growing need to develop more specialized programs for this population.
Medicare Plans
An average of 65% of residents are on Medicaid and other supplemental plans and do not have access to traditional Medicare or have Medicare/Medicaid replacement plans.
State Medicare Reduction
There is fear that there will be further reductions in State Medicaid payments, growing Medicaid replacement plans that further reduce benefits and the quality and quantity of care offered to the most vulnerable populations would deteriorate further.
Limited Services
Medicaid pays significantly less than other insurers and limits the amount of services that can be provided to these residents and in many states does not cover certain types of mental health services such as psychological care. This has resulted in many psychiatric and psychological providers either refusing to see or severely limiting the services provided to these residents. Ironically, these residents are statistically the most likely to exhibit behavioral disturbances or present with significant mental health issues and result in citations to facilities during annual survey, most likely to engage in resident to resident or staff violence, and lead to a higher percentage of litigation nursing homes face.
Critical Behavioral and Mental Health Services
Senior Behavioral Wellness Insurance Plan allows your facility to offer these resident’s greater access to critical behavioral and mental health services, proactive care, and services more at par with traditional Medicare coverage. SBW has the resources and clinical leadership to assist our participating facilities in reimbursing services to accommodate the unique needs of these populations.
Specialized Care Needs Are Growing
With the huge number of dementia and behavioral patients and the growing need for specialized care, it’s worth asking if the care people receive is actually at par or better than the care they would receive in a population of long-term residents with traditional Medicare coverage.
Enhanced Mental Health Benefits
Senior Behavioral Wellness Insurance Plans offer facilities the opportunity to provide enhanced mental health benefits for residents that are receiving only Medicaid or other replacement plans and can even the playing field in terms of the overall care received for your most at-risk population.
Overall Quality Rating
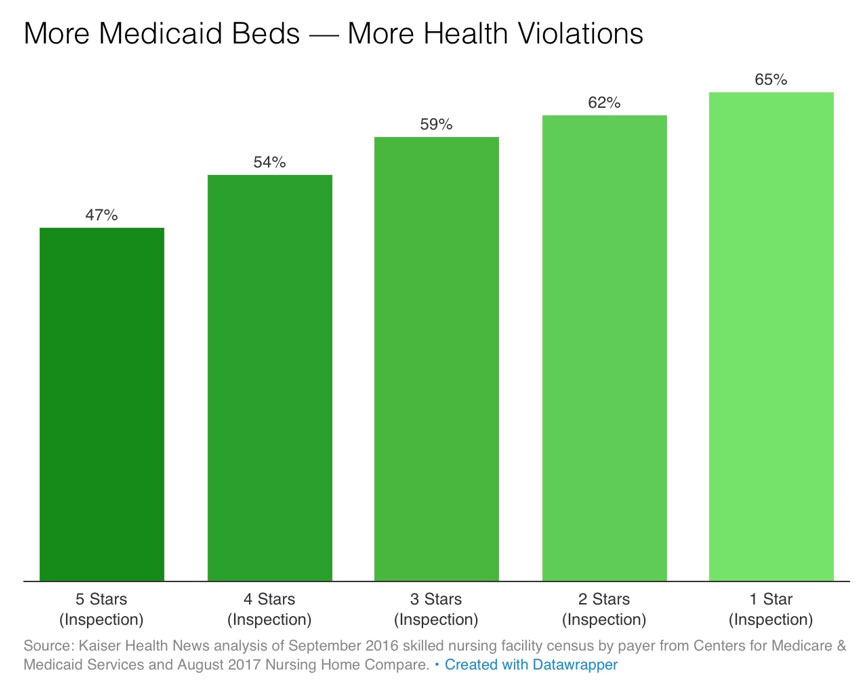
The government rates nursing homes on a scale from one to five stars, based in overall quality. One of the leading deficiencies that result in a lower star rating is how residents with mental health issues are cared for including use of certain classes of medications (particularly anti-psychotic use) which is highest amongst those on Medicaid due to limited availability of clinicians who can see these individuals or provide greatly reduced services due to reimbursement limitations.
The chart here shows how facilities with more health violations also have more Medicaid only beds.
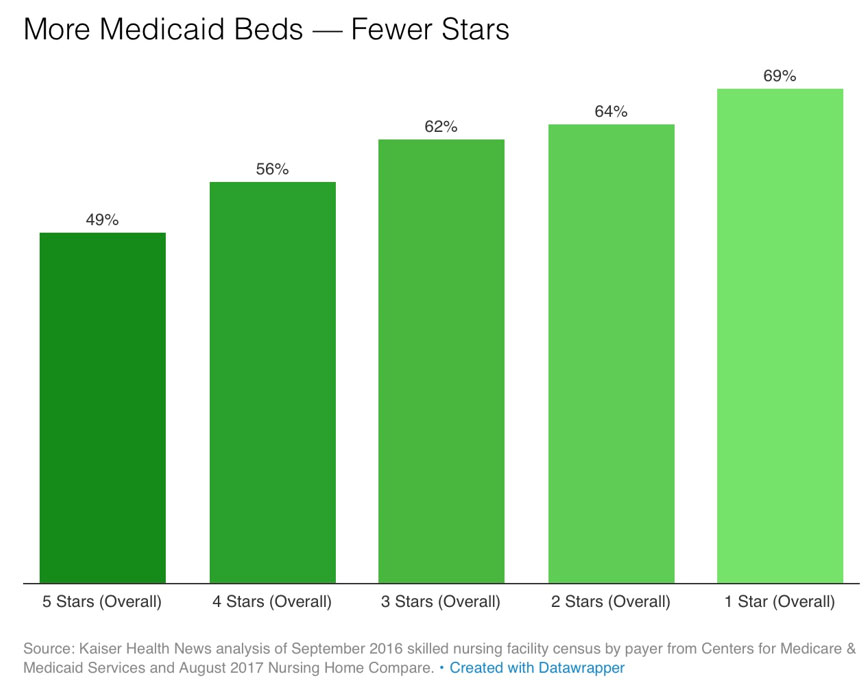
Fewer Star Ratings
The chart here shows the big picture: Nursing homes with higher percentages of residents covered by Medicaid earn fewer stars on the federal government’s quality rating system.
One-star homes average 69% of residents with Medicaid only; Five-star average 40% of residents on Medicaid only.
Better Quality Care & Improved Health Outcomes
A study out of the Department of Health Care Policy at Harvard Medical School discovered that dementia and mental health residents who resided in a long-term facility with enhanced mental health coverage for under-insured residents had better quality of care and improved health outcomes. More specifically, the study found that such facilities reduced inappropriate anti-psychotic use, physical or chemical restraints, pressure ulcers and exacerbation of other underlying medical conditions, hospitalizations, and the overall liability risk for the facility. In addition, facilities were able to accept a broader range of residents that otherwise would not have been admitted.
Full Access to Mental Health Care Professionals
We offer full access to mental health care professionals that can complement your existing team of care providers and mange this segment of the facility population or provide full facility coverage in those homes lacking adequate services, so the most vulnerable populations receive the highest level of care similar to those receiving Medicare and other private insurance benefits.
Long-term Dementia Study
Harvard researchers indicate that around 750,000 of the people living in a long-term care facility have a diagnosis of dementia-that’s half of all long-term care home residents.
